Healthcare facilities spend billions of dollars each year on administrative expenses. In 2019, it was estimated that a hospital would spend, on average, 31% of its total expenses on administrative tasks such as billing and insurance. In those days—before the pandemic and inflation made costs explode even higher—nationwide spending for healthcare administration was around $569 billion. Today, it’s likely those numbers have reached astronomical levels.
Some of the main drivers of that cost include the fees associated with having claims denied, as well as the employee hours needed to sort through patient documents, put together insurance claims, make corrections, and resubmit claims.
Thankfully, automation of the Revenue Cycle Management (RCM) process in healthcare facilities can solve all of these problems at once.
Automation cuts down on the time employees spend doing billing and insurance tasks, reduces the number of errors, and makes patient document processing instant and seamless.
Interested in adopting an RCM solution for your healthcare clinic or hospital? Read our RCM guide to brush up on the fundamentals.
Nividous is happy to put together a custom automated RCM platform for your facility. Get started right away by scheduling a demo.
FAQs About RCM Automation Solutions For Healthcare
What is the RCM workflow you’ll be automating?
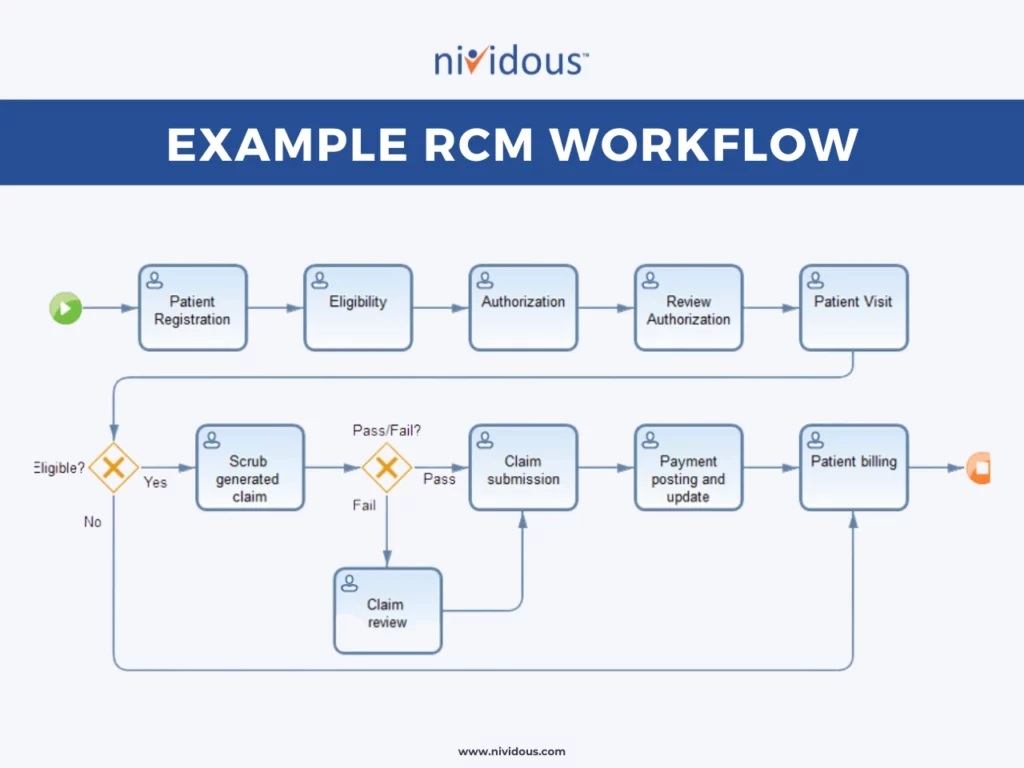
The specific steps within the RCM process may vary between different facilities and even for different patients, but it should encompass the entire financial flow from scheduling a patient all the way through receiving a payment for that patient’s visit. You can think of it as the whole financial process that goes along with operating a healthcare facility.
An example RCM workflow for a typical patient appointment looks something like this:
- Booking the patient’s appointment
- Filling out patient intake forms
- Checking the patient’s insurance eligibility
- Conducting the patient’s visit
- Preparing an insurance claim
- Submitting that claim to the insurer
- Receiving payment from the insurer
- Checking to make sure the bill has been paid in its entirety
- Sending invoice statements to the patient for the remainder of services that weren’t covered by the insurer
- Receiving payment from the patient
This flow may change if special circumstances arise. For example, some patients may need to see a specialist during the course of their treatment. If an elderly patient sees an eye doctor and gets a referral for cataract surgery, that patient’s RCM flow will expand to accommodate the extra steps of scheduling, pre-authorizing insurance coverage, conducting the appointment, and billing for the surgery consultation and procedure.
What’s the difference between RCM and healthcare billing?
The term Revenue Cycle Management is relatively new within healthcare settings.
A few years ago, most people referred to the financial process of running a healthcare facility as healthcare billing. As a result, some people use these terms interchangeably. However, they are not actually interchangeable; healthcare billing is a part of RCM rather than an alternative way to refer to the same thing.
While RCM includes all the steps from the very beginning interactions with a new patient—all the way back to scheduling the first appointment—healthcare billing concerns only the steps involved with getting paid for the patient’s visit.
Specifically, healthcare billing encompasses steps five through ten of the above example flow. It begins once the patient’s visit is complete and continues through the steps of preparing and submitting insurance claims, changing and resubmitting insufficient claims, receiving payments, and charging patients for portions not covered by insurance.
Can you automate the entire RCM process?
You certainly can.
Because RCM involves so many steps and requires some human oversight and educated decisions (the process of choosing a billing code alone is incredibly complex) it resists simple automation with robotic process automation (RPA) bots.
However, with a combination of RPA bots, AI technologies, and business process automation (BPA), you can automate the RCM process from beginning to end, dramatically simplifying and streamlining tasks for employees.
Here’s how Nividous would put together an example solution:
- Patient intake and registration: Most providers schedule appointments over the phone, online, and sometimes through a third-party call center. Nividous creates a simplified UI to make the scheduling process easier for online booking. If a patient can’t or doesn’t want to schedule their own appointment, we can also make this UI available to call center employees.The system can extract patient, provider, and insurance information from an uploaded image of the patient’s insurance card or previous patient charts. The information will be automatically entered into our standardized UI and will become the basis for automating all the future steps.
- Insurance eligibility: The system takes the entered information and checks it against the patient’s account within the insurance company’s portal. If a patient does not upload an insurance card and has no prior insurance information within the hospital’s records, the system can check for matching information within the portals of common insurance companies.Assuming the patient is covered, the system puts together a claim based on the patient’s intake information and the medical codes associated with their treatment. If a patient is not eligible for coverage, he or she will be asked to pay up front.
- Claim verification and submission: Using the data already gathered, the RCM solution verifies the accuracy of any insurance claims to ensure the lowest possible risk of claim denial. It then submits the claim automatically through the insurer’s website.
- Verification of transaction data: The RCM solution checks the details of insurance transactions and compares them to the hospital’s bank account statements to verify that the full amount has been paid. If there is a remaining fee, it assembles an invoice charging the patient for copays or services that were not covered.Once these fees have been paid, the system once again checks the accuracy of each transaction and ensures that the patient’s account shows $0 due. Once final payments are verified, the workflow is complete and the cycle can begin again with the next patient.
Throughout each of these steps, the automated system keeps the healthcare facility’s patient records up-to-date at all times. Before, during, and after the appointment, the physician and administrative workers will be able to conveniently access the patient’s medical records, insurance information, and all other important details within the automatically updated EMR portal.
How will the facility benefit from RCM automation?
Automating the RCM process provides similar benefits to automating any other complex business workflow. Automation saves time, frees employees to do more valuable tasks, reduces error, and improves efficiency.
By adopting an automated RCM solution within your healthcare facility, you can expect to see:
- A reduction in errors
- Fewer denied claims
- Faster processing times for claims
- Higher patient satisfaction
- A lighter load on facility staff
- Dramatic time savings
- Increased capacity for handling more patients
One previous Nividous client increased patient appointments by 300%, saved 37,000 employee hours, and saw a nine-day reduction in the average lag time between submitting a claim and receiving payment.
If you apply those results to your own facility’s numbers, you can estimate how much you might save with RCM automation.
Let Nividous automate your healthcare facility.
Along with RCM solutions, there are several other useful applications for AI in healthcare, such as predictive analytics and the automation of administrative tasks. Automate your hospital or clinic with a Nividous solution and tap into benefits like increased revenue and significant cost savings.



![The Path Forward for Intelligent Automation [2024 Trends] Blog Feature](https://nividous.com/wp-content/uploads/2024/05/The-Path-Forward-for-Intelligent-Automation-blog-feature-1.webp)
