Hospitals are currently facing a massive increase in their expenses, thanks to rising inflation and other factors. But inflation aside, providing top-of-the-line patient care has always required advanced medical equipment, phenomenal staff, and a system that incentivizes physicians, nurses, and administrative workers to consistently give their best effort.
There is no single solution capable of reducing costs across the board, but there are targeted approaches that can provide significant relief. Better still, you can implement those solutions without sacrificing patient care or staff satisfaction, and you’ll likely even improve them. One such strategy is to employ intelligent automation. Administrative costs in healthcare represent a significant chunk of expenses, which is why this tactic is so impactful.
Ready to Transform Your Business with AI, NLP, and Automation?
Watch our on-demand webinar and discover how AI, NLP, and advanced cutting-edge automation technologies can supercharge your growth, streamline processes, and reduce costs.
The Argument For Automating Administrative Costs In Healthcare
The Center for American Progress reported in 2019 that billing and insurance accounted for about 31% of total administrative costs in healthcare organizations nationwide. That 31% of admin expenses amounted to an estimated $569 billion — and that was in 2019, before the pandemic ravaged the healthcare system. Today’s numbers are probably far higher.
Under that umbrella of billing and insurance costs, we find that insurance claims soak up, on average, 13% of physician care costs and around 8.5% of a hospital’s total care spending. You can use these figures to estimate your hospital’s insurance spending if you want a more personalized number.
To make matters worse, hospitals aren’t just paying for successful insurance interactions. Denials can rack up charges very quickly, amounting to approximately $118 for every denied claim. That means every medical coding error results in a direct cost to the hospital. Combine these losses with those that stem from inefficiency with patient scheduling, payments, and other admin duties, and the full problem begins to come into focus.
To cut down on these astronomical costs, hospitals are starting to turn to automation, backed by advanced AI, as a way of reducing coding errors and eliminating the need for humans to busy themselves with these tasks. The idea is to free up hospital staff to provide better patient care. This comes with a clear benefit to the patients and staff, but it also means hospitals will cut down on the massive costs associated with paying human workers to handle billing, coding, and insurance tasks.
Despite these advantages, many hospitals and clinics have not yet leveraged this cost-saving strategy. When human lives — and billions of dollars — hang in the balance, the stakes of getting an automation system exactly right can feel much higher. This pressure can result in disagreements, politics, and delays that can stand in the way of implementing a solution that can help you to realize these benefits. At Nividous, we understand what’s at stake, because we help healthcare organizations achieve their automation goals every day. Nividous has seen healthcare organizations save up to 90% or more of certain admin costs, which represents a staggering amount in light of current spending estimates.
Nividous has seen healthcare organizations save up to 90% or more of certain admin costs, which represents a staggering amount in light of current spending estimates.
We may be reaching a point where hospitals can’t afford not to automate. Let’s discuss how your hospital or clinic can implement an intelligent administrative automation solution and take a look at some of the results you could expect to see.
Ready to move forward with a personalized automation solution for your healthcare organization? Request a demo with Nividous to get started.
How To Use AI To Lower Administrative Costs In Healthcare
Though every company’s situation and needs are unique, most healthcare admin solutions can be devised using a standardized framework. That doesn’t mean every solution will be the same; quite the opposite, in fact.
That’s because this framework helps us dive deeply into a company’s existing workflows to identify specific processes that can be improved with automation. The end result is a highly customized, AI-powered automation solution that works with your organization’s priorities and protocols.
This framework is best known by an acronym: ISUMO.
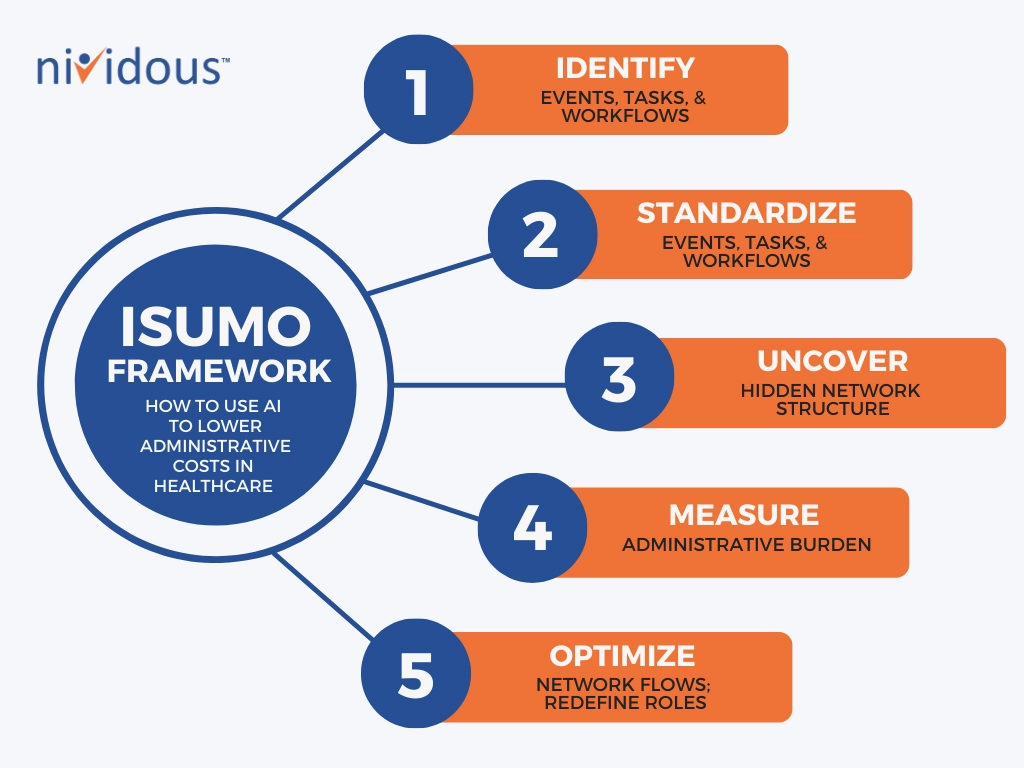
We’ll walk through each step of the ISUMO framework as described by the NEJM and explain how Nividous (or your own organization, if you choose to go your own way) builds customized healthcare admin automation programs layer by layer.
1. I: Identify events, tasks, and workflows.
Healthcare administrative workers deal with a huge volume of information on a daily basis. Staff may receive patient files from an external hospital, ask patients to fill out forms, or have multiple conversations with patients upon intake and during the course of treatment. In some cases, patients may have interacted with a chatbot before coming into the hospital in person.
Each of these interactions results in a massive amount of data, much of which takes the form of narrative text — a story told by the patient, or a description written by a physician in the patient’s charts, for example.
Rather than sorting through the data by hand, we use natural language processing (NLP) to identify the common threads and weave together the various conversational flows into a larger picture.
From there, hospital staff would normally have to perform certain actions with the information. They might submit an insurance claim, update a patient’s chart to reflect a medication change, or process outstanding payments.
These are all examples of workflows, and these workflows are what we’ll be seeking to automate.
Some tasks and events are straightforward; for example, many electronic health records systems function similarly, requiring specific actions to assign a diagnosis or make a medication change. Others may be murkier. Uncovering the inner workings of less-than-obvious workflows takes place during the second step.
This step is often referred to as process mining, and it can be done manually or with digital tools that can help identify tasks and piece together workflows.
2. S: Standardize system events.
Each workflow normally requires a human worker to complete a series of tasks to bring about an end result. Submitting an insurance claim, for example, consists of several steps including obtaining a physician’s diagnosis, searching patient records for relevant background information, identifying the correct medical code, inputting all the data into a submission form, and often answering questions from the insurance company after they’ve reviewed the file.
To automate a complex workflow like this, we must separate out each individual task and understand why and how it happens. The end result should be an outline (or several outlines) of which events must occur, and in what order, for the series of tasks to be successful. This outline, which often resembles a complicated flowchart, will be a helpful guide during the coding and customization portions of the automation process.
If the idea of mining through each workflow to build a logical flowchart of tasks and events sounds intimidating, don’t worry. If you work with Nividous, we will mine your processes for you and highlight the instances where automation seems to be the natural solution.
3. U: Uncover hidden network structure.
Different organizations — and different departments within one organization — share information using paperwork. Claims processing, patient scheduling, billing, and file transcript requests all require transmitting files from one place to another through a network of some sort. To automate these processes, we must understand which files are traveling where, why they must go there, and when this transmission should happen during the overall workflow.
It can be helpful to visualize informational networks in a graphical representation, so each connection and interaction is easily apparent. Thoroughly plotting the network structure in this way allows us to understand which team members are responsible for which tasks, and how frequently they must take certain actions.
4. M: Measure administrative burden.
How would you know how to lower administrative costs in healthcare if you didn’t know what your starting costs were and which were the areas that needed the most improvement? Once the tasks, network, and overall workflows have been carefully examined, it’s possible to measure the burden — in terms of financial costs, time spent, and other factors — of individual workflows.
This allows us to choose the solutions that would result in the biggest efficiency increases, the most time and money saved, and the highest level of satisfaction for the staff members who must interact with the platform every day.
The goal is to prioritize the automation of the most burdensome workflows first. These are the activities that weigh heavily on human workers and lead to mistakes, fatigue, and wasted time. Often, this means repetitive, tedious tasks are the first to go.
5. O: Optimize network flows and redefine roles.
If administrative workers didn’t have to waste time doing tedious paperwork and manually submitting claims, what else could they do with their time?
Many organizations focus on the direct benefits of automating workflows, such as the time and money saved. However, it’s wise to have a plan in place for those workers who now have a lot more free time on their hands. Ideally, these workers should redefine their roles to focus more heavily on providing compassionate patient care rather than dealing with insurance claims and paperwork.
Additionally, we often turn up other inefficiencies during the course of mapping out workflows and network structures. Even if a particular component doesn’t rank highly on the priority list for automation, it can certainly be redefined and restructured with efficiency in mind.
Case Studies That Illustrate What You Can Achieve By Automating Administrative Tasks
One organization reduced insurance claim denials by 90% with automation from Nividous.
The problem: Every insurance claim has an associated medical encoding that varies by the type of disease, the treatment needed, and other factors. Submitting a claim manually meant employees had to comb through pages of narrative text on each patient’s chart, pick out the relevant details, and submit the claim without making any mistakes or missing anything important. To put this task into perspective, knee surgeries alone may fall under a few hundred different medical codes. Identifying the correct one, time after time, for patient after patient, was cumbersome to say the least.
This client was incurring too many insurance claim denials as a result of the complexity of these tasks.
The solution: Nividous used NLP to interpret the text in each patient’s chart, identifying keywords and synonyms that provide clues as to what the correct medical code should be.
The result: Using this automated process helped the organization eliminate 90% of insurance claim denials.
Another organization reduced the need for manual data extraction in patient charts by achieving 94% accuracy with an automated Nividous solution.
The problem: Many healthcare organizations still rely on bulk-packaged PDFs sent over a fax system to transmit patient files and forms. For this client, each bulk PDF contained up to 73 different types of patient forms and often came to thousands of pages in length. Reading, classifying, and extracting relevant data manually from such an enormous source was a monumental task for their employees to complete, and such overwhelming tedium tends to increase error rates for fatigued workers.
The solution: Using automation from Nividous, this organization implemented a solution that downloads these massive document packs from shared directories, reads them, extracts patient information and important form data, and sorts the information based on the patient’s info and the document type. These results are then uploaded automatically into the organization’s health records system.
The result: With a bare minimum of 750 monthly faxes sent — and sometimes over 1,000 — this company saves at least 163 employee hours and $3,267 every month.
How much could you potentially save with a Nividous automated solution?
Every increase to efficiency widens margins by reducing costs or boosting income potential. Because so many variables are involved, it can be difficult to predict the exact dollar amount you might save by automating your healthcare admin processes.
However, sometimes our previous clients can retrospectively give us hard numbers that illustrate their results from our automation solutions.
For example, AEG Vision saves $75 million every year in claims payments alone. And another specialty healthcare company saw a 45% decrease in their operational costs after automating patient data extractions and claim submissions.
For a more personalized estimate, you can use this ROI calculator with your organization’s specific information.
Which healthcare admin tasks weigh most heavily on your organization?
You may already know the answer to this question, or you may have only a vague idea that automation could greatly improve your workflows. Regardless of your starting point, Nividous can help guide you along the path toward a customized, fine-tuned automation solution that will dramatically cut down on your need for manual administrative tasks.
Contact Nividous to schedule a demo and see what automation could do for your healthcare business.